A Runner’s Story
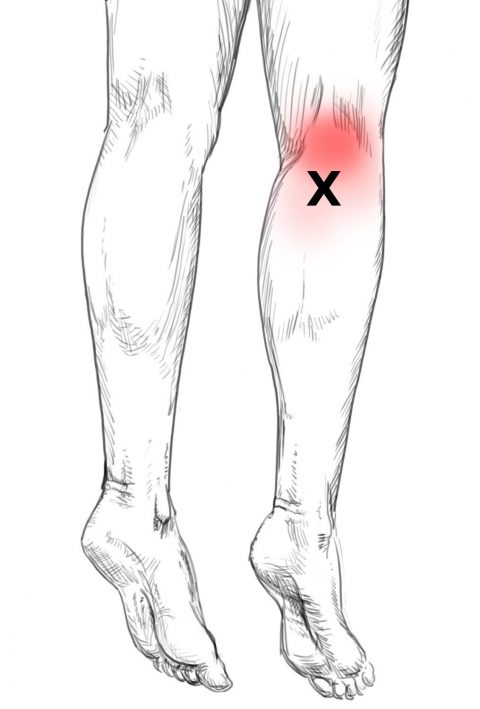
A runner training for his first 5k recently came in due to pain on the bottom of his foot, self-diagnosed plantar fasciitis. He noted that it was worse in the morning, especially during the first few steps. He was currently wearing custom orthotics and brand......